OSTEOSARCOMA
- Hits: 2108
Osteosarcoma is the second most common cancer of the bone. It occurs in 4-6 patients per million each year.
Most cases of osteosarcoma are spontaneous, which we call primary, but rarely secondary, which we call Paget’s disease or radiation. Some syndromes (hereditary retinoblastoma, Li-Fraumeni, etc.) can create a genetic predisposition to the development of this cancer. Secondary osteosarcomas are more aggressive and have a poor prognosis.
The most common type of primary osteosarcoma is the classical osteosarcoma. Other types such as telangiectatic, parosteal, periosteal, small cell, high-grade superficial are also found.
Although classical osteosarcoma can be seen at very early and late ages, the most common age range is 10-25 years. It is most commonly found around the knee and shoulder. It is slightly more common in males. It is often found in the metaphyseal region of the bone.
Osteosarcoma patients usually present to the hospital with pain. The pain is often caused by bone destruction. While the pain is mild at first, it increases over time, becomes persistent at rest, and does not respond adequately to pain medication. It is common for these patients to be awakened at night by the pain. The other most common complaint is swelling. Because of these two complaints, the patient begins to have difficulty using the limb where the tumor is located.
Laboratory tests of osteosarcoma patients may show elevated alkaline phosphatase, lactate dehydrogenase, and sedimentation rate. The initial radiologic evaluation is a direct radiograph.
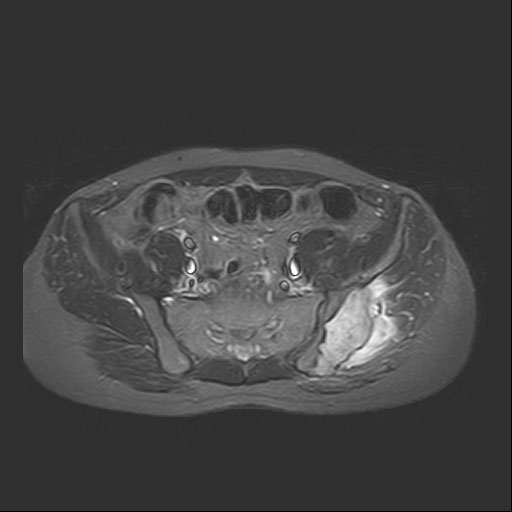
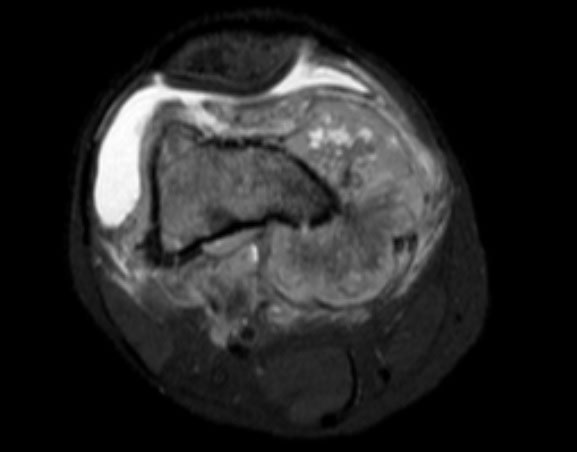
Radiologic evaluation of patients with osteosarcoma begins with plain radiographs. In the direct radiograph, destruction and construction (periosteal reaction: Codman triangle, sunburst) are seen together in the bone where the tumor is located. It is a heterogeneous mass with indistinct borders. Tomography shows the bone destruction more clearly. Magnetic resonance imaging shows the soft tissue component of the tumor and its borders more clearly. MRI is also helpful in assessing response to chemotherapy and planning surgery. We also use MRI for follow-up.
In patients with suspected osteosarcoma, a biopsy is performed to confirm the diagnosis after clinical and radiologic evaluation. The biopsy can often be performed using the closed-needle technique. It is important that the physician who performs the biopsy procedure is an orthopedic oncologist who specializes in bone and soft tissue tumor surgery, and the physician who performs the microscopic examinations is a specialist in bone and soft tissue pathology.
Patients diagnosed with osteosarcoma should be evaluated for the presence of proximal (lymph node, skip metastases) and distant (lung, other bones) metastases using various tests (lung and abdominal CT, whole-body MRI, whole-body bone scintigraphy, or PET-CT).
The classical treatment of osteosarcoma (except for parosteal osteosarcoma) is 3 cycles of chemotherapy (different combinations of Adriamycin (Doxorubicin), Cisplatin, Methotrexate, Ifosfamide drugs can be applied) followed by surgery to remove the tumor cleanly (wide resection) and then 3 cycles of chemotherapy again. The surgery aims to preserve the patient’s limb and the removed bone or joint is reconstructed with biological (recovery, fibula, allograft, etc.) or non-biological (prosthesis). Tumors that are not removed cleanly with wide margins have a recurrence rate of almost one hundred percent and are prone to metastasis. It is therefore essential that the surgeon performing the operation is an orthopedic oncologist with experience in this field. A pathological fracture does not require amputation (removal of the patient’s limb).
Because osteosarcoma is resistant to radiotherapy, it is not used in routine treatment. However, radiotherapy can be used for palliative purposes in metastatic tumors.
The 5-year survival rate for patients with osteosarcoma is 60-70%. The presence of metastases (including skip lesions), high grade, poor response to chemotherapy (<90% necrosis), pelvic, spinal localization, >10 cm in size, presence of pathologic fracture, male gender and elevated ALP may negatively affect this rate.
Osteosarcoma patients should be followed for many years after treatment for recurrence and metastasis.