Spinal Metastasis (Cancer Spread to the Spinal Bones)
- Hits: 322
Spinal metastasis is the spread of cancer from internal organs to the spinal bones, often causing back pain and other symptoms. Early diagnosis and tailored treatments are crucial for enhancing the quality of life and managing symptoms effectively.
What is Spinal Metastasis?
It is the spread, or metastasis, of cancer from the internal organs where it originated to the bones of the spine. This spread generally occurs through the bloodstream, although it can also spread via the lymphatic system (as with breast, prostate, and testicular cancers) or through direct proximity (as with lung cancer). Spinal metastasis is the most common malignant tumor of the spine. It typically occurs after age 40 and indicates that the existing cancer has reached an advanced stage (stage 4). Such patients should be evaluated in a multidisciplinary approach (Orthopedic Oncology specialist, Medical and Radiation Oncologists, Pathology, Radiology, and Nuclear Medicine).
How Common is Spinal Metastasis?
In our country, approximately 240,000 people are diagnosed with cancer each year. In recent years, as cancer treatments have advanced and life expectancy has increased, the incidence of spinal metastasis has also risen. After the lungs and liver, bone is the third most common site of metastasis. Depending on the type of cancer, spinal metastasis can occur in approximately 40% of cases.
What Causes Spinal Metastasis, and Which Cancers Most Frequently Spread to the Spine?
The cause of spinal metastasis is cancers originating in other organs. Any type of cancer has the potential to metastasize to the spinal bones; however, breast, prostate, lung, kidney, and thyroid cancers are the most likely to spread to bones. This is because these types of cancer are more prevalent in the population, and the expected lifespan of these patients is relatively long.
What are the Symptoms of Spinal Metastasis?
The most common and initial symptom of spinal metastasis is back or lower back pain. Persistent pain even during rest and an increase in severity over time are typical. Patients may eventually wake up from sleep due to pain at night and may not find sufficient relief from standard pain medications.
Patients may infrequently (10-30%) present to a doctor due to spinal fractures caused by the weakening of the bone due to metastasis.
Patients with spinal metastasis (20-30%) may also experience numbness, tingling, or weakness in the arms or legs due to compression of the spinal cord or nerve roots. Patients may have difficulty walking, and nerve damage may lead to impaired bowel and bladder function. In particularly delayed cases, partial or complete paralysis may develop due to compression of the spinal cord by bone fragments from fractures or by the advancing tumor.
How is Spinal Metastasis Diagnosed?
Patients with spinal metastasis can present clinically in various ways. Typically, it is detected either during routine screening for a patient with a known cancer diagnosis and treatment or when a patient consults a doctor due to the symptoms mentioned above. In some cases, spinal metastasis may be the initial diagnosis even in the absence of a prior cancer history. Additionally, it may present as a sign of previously treated cancer that reappears years later.
Diagnosing spinal metastasis is of vital importance. It is essential to differentiate between a tumor originating directly from the bone and the patient's existing tumor to avoid irreversible errors that could seriously impact the patient’s life. For this reason, after a detailed patient history, physical examination, and necessary imaging tests, a biopsy may be needed in some cases.
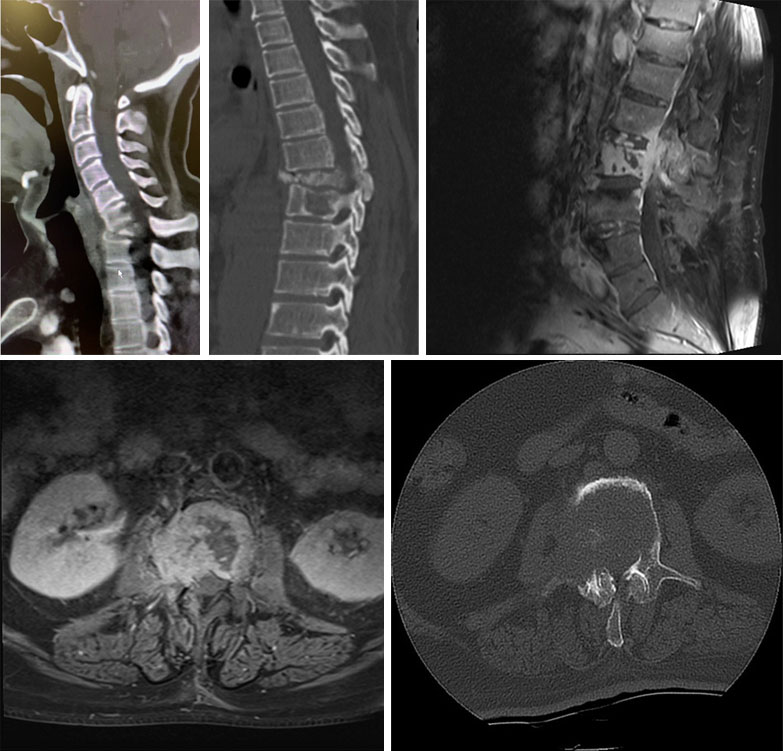
The most basic test is a two-view X-ray of the affected bone. CT scans can provide a better understanding of bone destruction, while CT scans of the chest and abdomen may be taken to locate the primary cancer site in cases of metastasis of unknown origin. For soft tissue evaluation and especially to detect spinal cord compression, contrast-enhanced MRI is the best method.
In spinal lesions identified in patients over 40, laboratory tests for tumor markers may be requested if metastasis is suspected.
If the patient has no history of cancer or if a single spinal involvement is identified through nuclear medicine techniques (PET-CT or Scintigraphy) during screening, a biopsy may be performed. Biopsy is usually conducted as a closed procedure with special needles under imaging guidance.
Despite all efforts, the source of the tumor cannot be determined in 3-4% of patients.
Can Spinal Metastasis Be Confused with Other Diseases, and How Can It Be Distinguished?
Spinal metastasis can often be mistaken for other spinal disorders, particularly those causing pain and nerve compression symptoms, such as worn-out spine conditions (e.g., herniated discs, spinal stenosis). This is primarily because these conditions share common symptoms.
Similarly, osteoporosis—a bone-thinning disease—is another common cause of spinal fractures, particularly in the same age group.
Distinguishing between these conditions requires experience, as well as meticulous clinical and radiological evaluation. Initially, a thorough patient history should be taken, and the possibility of a cancer history should be explored. Even if there is no known cancer history, laboratory tests and full-body screening should be conducted if suspicious circumstances are present. CT scans and MRIs of the spine should also be examined in detail.
Why is Early Diagnosis Important in Spinal Metastasis?
Early diagnosis of spinal metastasis is crucial for improving quality of life, enabling patients to resume daily activities, preventing potential spinal fractures and nerve damage, and guiding existing cancer treatments. Therefore, if a patient with a history of cancer experiences symptoms such as neck, back, or lower back pain that worsens over time and persists even at rest, it is highly recommended that they consult a specialist.
How is Spinal Metastasis Treated, and What are the Treatment Goals?
The primary goals in treating spinal metastasis are to relieve pain, prevent fractures, and improve patient function and quality of life. Factors that influence treatment decisions include the type and spread of the cancer, the extent of bone damage, the tumor’s responsiveness to radiotherapy and chemotherapy, the patient’s overall health, and their life expectancy.
Treatment can be categorized into three main approaches: medical (bone-strengthening bisphosphonates or denosumab, chemotherapy, hormone therapy, immunotherapy, and targeted drugs), radiotherapy, and surgery.
Medical treatment is administered and monitored by medical oncology specialists. Radiotherapy is the primary treatment choice for most cases of spinal metastasis and is planned and delivered by radiation oncologists. Additionally, radiotherapy is routinely applied post-surgery to reduce the risk of tumor recurrence.
Surgical treatment is particularly employed in cases of fracture risk or presence, or if there is compression of the spinal cord or nerve roots. Surgery may also be considered if pain cannot be controlled despite radiotherapy and medical treatments or if the tumor recurs. Surgical intervention may also be chosen to remove the tumor if it is resistant to radiotherapy, such as with kidney and thyroid cancers, or in cases of solitary spinal metastasis.
Depending on the patient’s condition and the specifics of the spinal metastasis, both minimally invasive and open surgical methods may be used.
The Importance of Early Intervention in Preventing Fractures Caused by Spinal Metastasis
Fractures caused by spinal metastasis can negatively affect a patient's expected lifespan and daily living activities, making early diagnosis and intervention crucial. Addressing issues before fractures occur can reduce surgical risks, expedite the patient’s return to daily life, and minimize the need for additional surgeries. In cases of fractures due to spinal metastasis, vertebroplasty (cementing) or screw fixation may be applied, depending on the severity of the fracture (collapse degree, spinal curvature, spinal cord compression, etc.). The chosen method should ideally provide stability for the remainder of the patient’s life and minimize the need for further surgical procedures.
The most commonly used method in cases of metastasis to the spinal bones is vertebroplasty, a minimally invasive cementing procedure. This procedure can be performed under local anesthesia on an outpatient basis and provides rapid and effective pain relief. Patients can typically be discharged the same day. An added advantage is that multiple vertebrae can be treated in a single session if necessary, which strengthens weakened and collapsed vertebrae to prevent further damage.
In cases of severe vertebral collapse and spinal cord compression, open surgery may be required. In such cases, the tumor tissue and/or fractured bone fragments causing spinal cord compression are typically removed (decompression surgery), and the upper and lower vertebrae are stabilized with screws (instrumentation). In cases of severe or comminuted fractures, radiotherapy-resistant or recurrent cancer, and solitary spinal metastasis, a corpectomy may be performed to completely remove the affected vertebra and reconstruct the space with specialized implants (cage). In the presence of clinical symptoms caused by spinal cord or nerve root damage (especially sensory and motor deficits), a short-term steroid (cortisone) treatment may be administered in addition to surgery to reduce inflammation caused by the tumor and fracture.
What are the Latest Treatment Methods for Spinal Metastasis?
The latest methods for treating spinal metastasis involve minimally invasive procedures performed under imaging guidance (CT, portable X-ray) and anesthesia, such as radiofrequency ablation (RFA), microwave ablation, and cryoablation (freezing). Among these methods, radiofrequency ablation is the most commonly preferred.
Radiofrequency ablation (RFA) is a procedure that destroys the tumor by heating it to high temperatures in a minimally invasive manner. It can be safely applied to multiple bones, including the spine, and is an effective method with low risk and quick results. An added advantage is that it can be used in radiotherapy-resistant or recurrent (relapsed) spinal metastases. In selected patients, a cementing procedure can be safely performed after radiofrequency ablation through the same entry point.